The Business of Codes
Why there are so many diagnoses in the chart
Most people believe that a medical diagnosis represents some underlying biological truth. There’s a term in the chart, it’s on all the paperwork, it even has it’s own code associated with it.
This isn’t reality, though. As an example, take this fictionalized case of Ms. Hess. She’s recovering well from her ruptured intracranial aneurysm six months ago, nearly back to normal, just occasional headaches and some “brain fog.” Considering how catastrophic a ruptured aneurysm can be, she’s fortunate and knows it.
She pulls up her chart on the patient portal and asks why she’s listed as having both a traumatic intracranial hemorrhage and a non-traumatic one. It makes no sense. I agree, rolling my eyes. I explain how diagnoses get layered onto charts and how we doctors have almost no ability to clean them up. Ms. Hess now carries 28 separate diagnoses. Her story is classic: she was walking down the dairy aisle when she collapsed. Some assumed she slipped. EMS found her conscious but delirious. In the ER, the doctor, rushing to order a CT, entered “fall” as the required diagnosis code to get the scan approved.
When the scan showed blood in her brain, he coded traumatic intracranial hemorrhage. She had fallen; the blood must have come from trauma. But when neurosurgery was consulted, the pattern was unmistakable: aneurysmal subarachnoid hemorrhage. The vessel burst first, causing her to fall. Aneurysmal bleeds have a distinct CT appearance that is different from traumatic ones. An ER doctor isn’t expected to spot that. So, I admitted her under the correct code: non-traumatic intracranial hemorrhage (I60.9, nontraumatic subarachnoid hemorrhage, unspecified). Yet all three codes (fall, traumatic bleed, non-traumatic bleed) remain in her record forever. She also picked up a hospital-acquired urinary tract infection, protein-calorie malnutrition, and delirium. Those live there too.
Now, in clinic, she mentions low back pain shooting down her right leg. I also have expertise there, so I know it’s lumbar foraminal stenosis at L4-5 from facet arthropathy causing radiculopathy. But because she’s complained of this to primary care, the ER, and pain management, her chart also lists lumbar stenosis, lumbar herniated disc, sciatica, lumbar degenerative disc disease with claudication, and plain “lumbago.” Which is it? Nobody knows. The chart is a patchwork of whatever code got the MRI approved, the injection authorized, or the surgery paid for.
The same stacking happens everywhere. COPD: one note says J44.9 (unspecified), the ER adds J44.1 (with acute exacerbation) for a flare, and the pulmonologist throws in J44.0 (with acute lower respiratory infection) because the patient had bronchitis. Diabetes? The primary care doctor codes E11.9 (type 2 without complications). The endocrinologist adds E11.40 (with diabetic neuropathy). The podiatrist codes E11.621 (with foot ulcer) for the wound clinic referral. These aren’t lies but rather compliance in a system that demands a code for everything.
Yes, the doctors could go back through and clean her diagnosis list up, but nobody wants to take responsibility for that. The primary care doctor isn’t qualified to determine which lumbar spine code is the right one to keep in the chart. Plus, as many doctors routinely point out, they have become data entry clerks. Data already show that doctors spend 2 hours on the computer for every hour of patient care time. No patient wants their doctor spending even more time cleaning up messy data when they could be having more face to face time. There’s no incentive for doctors to clean up the diagnosis list.
CMS requires diagnosis codes for every order, every billable visit, every procedure. The current version is ICD-10-CM, maintained by the WHO but expanded in the United States to more than 74,000 diagnosis codes.
These codes mandate a granular, but ultimately useless level of detail. You can’t just write “heart failure.” You need systolic or diastolic, acute or chronic, left ventricular or combined: I50.23 (acute on chronic systolic), I50.33 (acute on chronic diastolic), I50.43 (acute on chronic combined). A neurosurgeon or orthopedic surgeon isn’t expected to know the precise diabetes subtype, yet the system demands it. That’s why the same degenerative-disc patient ends up with four near-identical low-back-pain codes: one for the MRI referral, one for the pain injection, one for the ER visit, and one for the surgeon’s pre-op note.
The incentives go beyond insurance approval. During the COVID pandemic, the CARES Act added a 20% boost to the hospital’s DRG payment for any discharge that included the COVID diagnosis code U07.1. Now, when a code is that heavily incentivized, rational actors will respond. Hospitals tested everyone, trauma patients, car-accident victims, elective admissions. A positive PCR (which often picked up minute levels of virus in non-infected people), even asymptomatic or incidental, triggered the bonus. The public debate was brutal: patients were counted as “COVID hospitalizations” whether the virus caused the admission or not. Studies during the Omicron wave found 10–25% (and in some hospitals higher) of COVID-positive inpatients were incidental, admitted for something else entirely. Yet, because of the incentives, no hospital would dare exclude a COVID diagnosis if they had the opportunity to get the payment boost.
At least COVID had a lab test. Plenty of diagnoses do not. Concussion is clinical, with no reliable biomarker, and no imaging requirement for mild cases. Autism spectrum disorder rests on behavioral observation and developmental history; no blood test or scan confirms it. Chronic fatigue syndrome (ME/CFS) is symptom-based and exclusionary. Fibromyalgia relies on widespread pain and tender points. Irritable bowel syndrome follows Rome criteria after ruling out other causes. Major depression, anxiety disorders, and ADHD are all syndromic. That does not mean these conditions are imaginary. It means they lack the kind of objective boundary that makes them resistant to incentive distortion.
Even when objective tests exist, they are often ignored. A large UK study of more than 14,000 primary care patients coded with COPD found that only 52% had consistent airflow obstruction on repeated spirometry confirming the diagnosis. Another 11.5% had no obstruction at all on multiple tests, yet many continued receiving inhalers.
To see how the incentives play out, look at what an Autism diagnosis can generate. When a diagnosis unlocks hundreds of thousands of dollars in services, the diagnosis will proliferate. In Minnesota, the Medicaid autism program (Early Intensive Developmental and Behavioral Intervention, or EIDBI), saw providers balloon from 41 in 2018 to 328 in 2024, a 700% jump. Payments exploded from roughly $6 million to nearly $192 million, a 3,000% increase. Federal investigators found fake diagnoses, billing for services never delivered, and kickbacks to parents. One provider alone extracted $14 million. Audits flagged 90% of recent claims as non-compliant in some reviews. Across related Minnesota human-services programs, prosecutors estimate half or more of the $18 billion spent since 2018 may have been fraudulent. Are there children for whom these services are needed? Of course. But this is a clear example of the rich incentives that come with an arbitrary “autism” diagnosis.
Ultimately, this system is used by CMS to control what doctors can do. Try ordering an MRI on a patient whose chart has the “wrong” code and the EHR blocks it. The software helpfully lists “approved” diagnoses, forcing the physician to comb through and find the closest one to reality to get the test approved. Multiply that by 20–50 patients a day and you’re burning hours on documentation instead of thinking about the human in front of you.
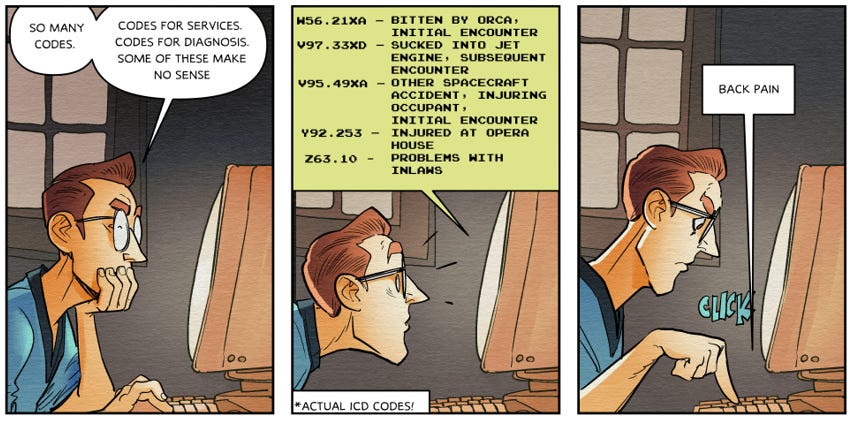
There are even absurd diagnosis codes that reveal how ridiculous the system has become:
Z63.1 – Problems in relationship with in-laws
W56.21XA – Bitten by orca, initial encounter
V97.33XA – Sucked into jet engine, initial encounter
Y92.253 – Opera house as the place of occurrence of the external cause
These aren’t jokes. They’re real, billable codes. They reflect a system that is cumbersome, needlessly granular, and ridiculous. The system demands extraordinary specificity for common conditions and devotes the same infrastructure to orca bites and jet engines. We covered this in volume 1 of Claim Denied.
One argument for all this granularity is “data tracking.” Yet, because of all the misaligned incentives above, the data are often worthless. When diagnoses are shaped by billing incentives rather than biological reality, the dataset ceases to reflect disease prevalence. It reflects reimbursement rules. In one large analysis of patients like Ms. Hess, 40% carried both traumatic and non-traumatic intracranial hemorrhage codes despite a clear etiology. Any study trying to investigate outcomes or clinical course around either head trauma versus aneurysm rupture is contaminated by a large cohort of patients with both diagnosis. The truth is buried under contradictory codes.
This is gatekeeping by diagnosis code. Central planners decided that every clinical thought must be translated into their language, then used that language to ration, reward, and punish. The result is a chart full of contradictions, care distorted by incentives, and physicians turned into data-entry clerks. The patient gets lost in the codes. And the system keeps demanding more specificity because in a centrally planned healthcare economy, the planner’s need for control always outweighs the clinician’s need for clarity.


The codes and arbitrariness of the system are designed not to deliver better care but to ensure higher profits for insurance companies. Delay and denial are a feature, as they say, not a bug.
Here was my take a few months back....I am not a bot. I get a lot of bot comments..https://open.substack.com/pub/danjschmidt/p/coding-mastodons-doctor-story?utm_campaign=post-expanded-share&utm_medium=web